Adopt and Adapt: Draw from Other Fields and Tailor to Fit Your Program
When Mark Paglia became director of a small (15 person) Outpatient Services program at Providence Hospital, he recognized an unhealthy work culture and a system that was not operating efficiently. He worked with staff over the ensuing months to make changes that resulted in:
- A healthier and jovial environment
- Smoother administrative systems
- Improvements to the facility and tools of work
- Increased productivity
As one clinician put it, 'All our oars are rowing in the same direction, and if feels good."
How did they do it?
First, Mark listened. Over a period of two weeks, he interviewed each staff member for about an hour, asking:
- What motivates you to come to work? What do you enjoy?
- What things do you feel need improvement?
- What advice do you have for me in my new role as director?
He took about 20 pages of notes, and says, "About a half page was all the things that motivated people to come to work and the other 19 1/2 pages were things they wanted to improve!"
He organized the suggested improvements to create a tool he dubbed "The Prov Outpatient Workplan." He enlarged the plan to poster sized, brought it back to staff, and gave them five stickers each to identify their top priorities.
The number one priority was payroll errors - this small department had four different timesheets and four ways to submit them, and there were consistent issues with the pay every week due to mistakes in entering the information. A small workgroup met the very next week, designed a single timesheet, and implemented it. Payroll errors were eliminated.
Small workgroups addressed multiple items in parallel:
- Scheduling issues
- Assignment of individual clients from the many groups to case managers
- Training needs - updated the whole year's training schedule based on content staff felt they needed, engaging experts identified by staff
- Vacation protocol - staff decided how many people could be on vacation at the same time.
Staff own the changes, so staff implement the changes
Once staff set the training schedule and content, they participated at a very high rate, mostly 100% attendance. Before this change, arranging make-up trainings for those who missed had been a scheduling issue. Similarly, owning the decision about vacation protocol has made the policy easy to live with. Says Mark, "The more you involve folks, invite them into the process and to take ownership, the more compliance there is up front."
Two indications of how invested staff are:
-
All these results were achieved with existing staff. No staff left.
-
When the Senior Clinician, who functions as operations manager, was relocating, he gave four months notice - plenty of time to find a replacement and overlap with the new Senior Clinician to create a smooth transition.
Communication was increased and made more consistent:
- Weekly staff meetings replaced monthly staff meetings
- Individual supervision was implemented more consistently, and while it continued to focus on clinical material, supervision now also includes sharing administrative information that comes up between staff meetings.
Although one might think that the additional administrative time was taking away from clinical time, the program has actually been more productive.
- Workstations and computers were added for Per Diem staff
- Old phones were replaced, since the loud ring (which could not be modified) was interrupting groups.
Mark considers the up front and ongoing investment of both time and money key to saving time that had originally been spent working out payroll errors and scheduling issues, and making up for information gaps...and waiting in group for the loud phones to stop ringing. Facilities were the biggest expense, but many changes were made at no expense.
Five months after beginning the improvement process, staff started to involve clients in the work. This Intensive Outpatient program runs long groups, and clients identified a wish for coffee as well as facilities issues related to the comfort of the chairs and the room. So chairs were replaced and a coffee-maker was purchased, and now coffee is provided for every group.
Mark feels the "investment in healthy operations" was totally worthwhile.
Next Steps
After Year One of this work plan passed, a new Senior Clinician was hired. Mark planned to revisit using the same methodology, having this new staff member do the interviews. The goal is to continue to find out what still needs to be improved and what new items should be added.
Results
Mark says, "We are a fast-moving Outpatient clinic, and we are not perfect. But morale has dramatically increased, the culture has dramatically shifted to be enjoyable to work with, people are laughing and joking and there has been a dramatic improvement in teamwork."
The Change Process
Mark was familiar with the Efficacy Institute's Learning Model* (support for children's learning using a Self-Directed Improvement System) from his previous work in Springfield with Step Up Springfield; he also had recently taken a NIATx Fundamentals course when he started working with Outpatient Services.
He drew on both these models in deciding what steps to take to make things better. He describes the process that his program currently uses as:
- Raise an issue
- Brainstorm/Look at what was
- Update a draft of the policy or practice
- Bring it back to staff and make minor tweaks
- Set an effective date and notify staff
- Implement
- Revisit.
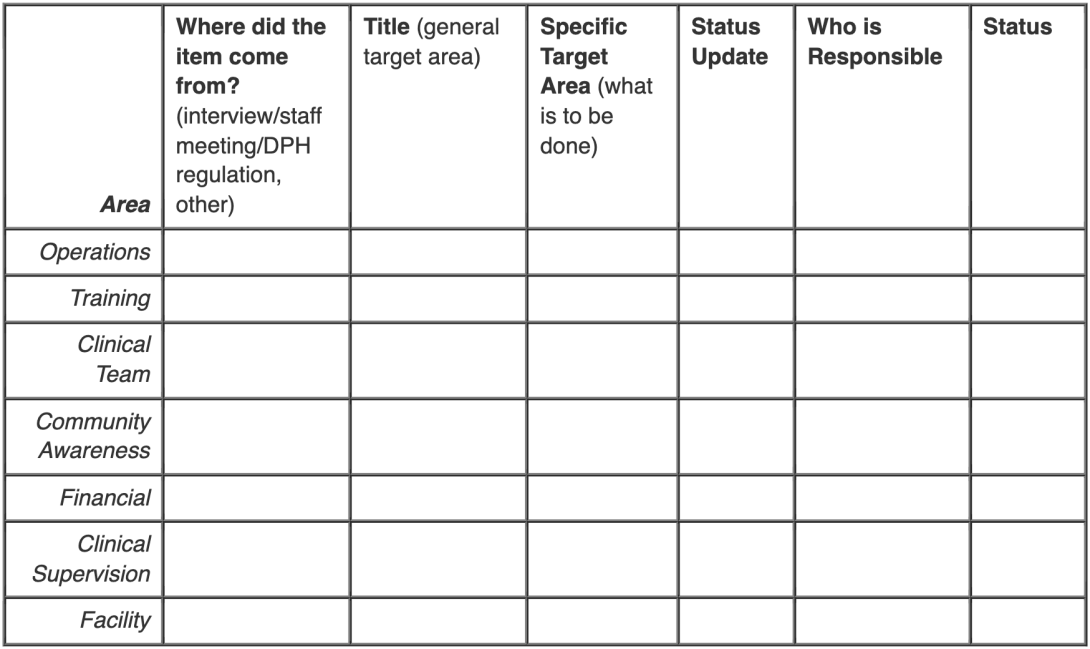
The Work Plan format looks like this:
*The general "Learning Model" Mark adapted, as he describes it, involved:
- Set a target
- Assess where you are
- Get data
- Ask "Why are we here, when we want to be there?"
- Create a plan to close the gap
- Carry out the plan
- Continue the cycle to reassess and ask "Why?" again